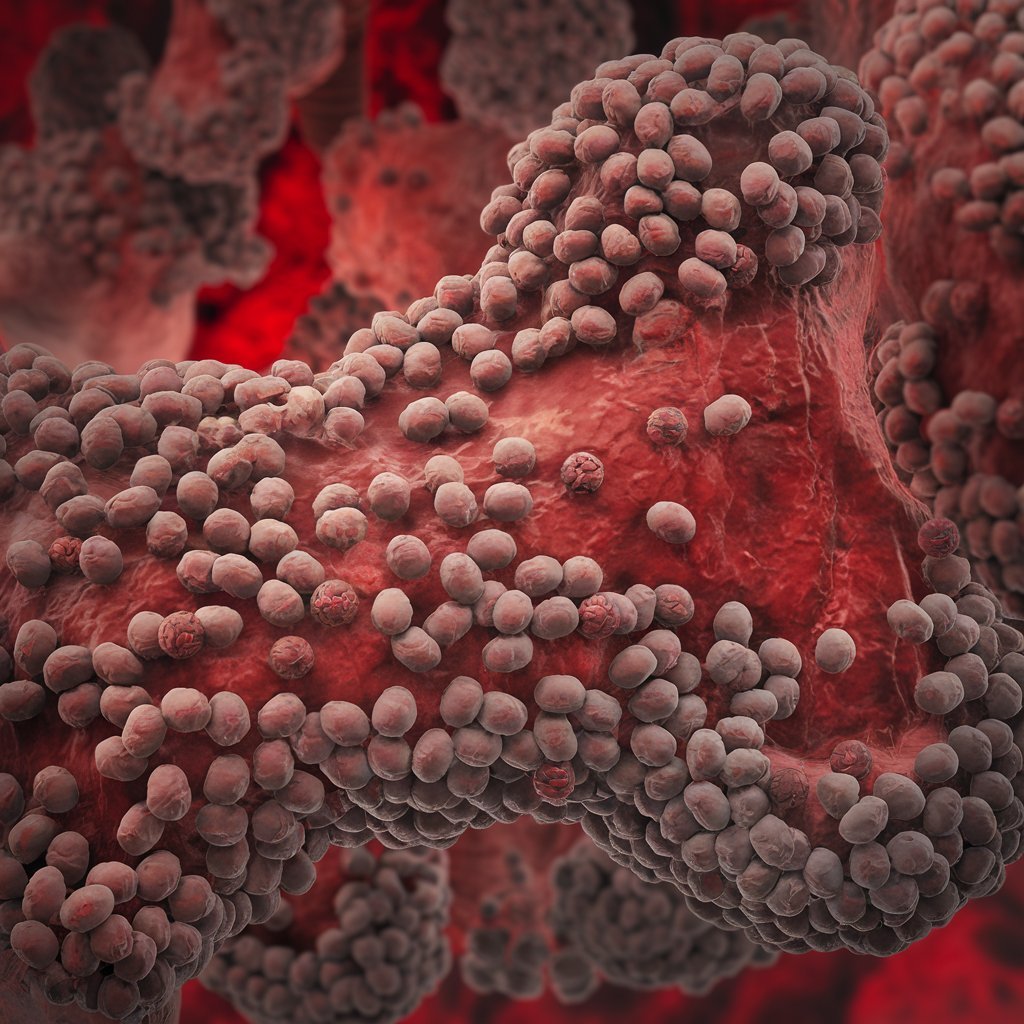
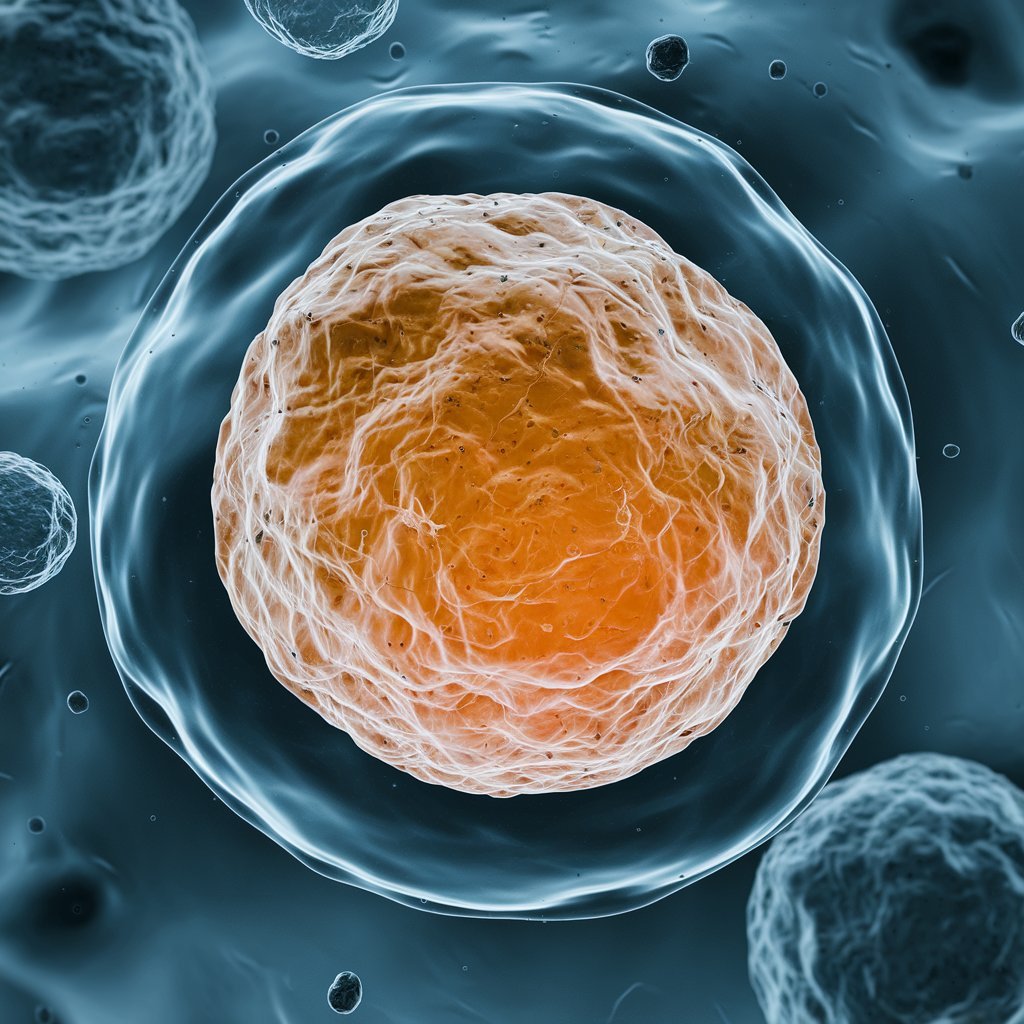
Hypereosinophilic syndromes (HES) are a rare group of blood disorders characterized by an abnormally high number of white blood cells called eosinophils. Eosinophils are crucial for your immune system’s response to infections and allergic reactions.1 In people with HES, chronically elevated eosinophil levels can infiltrate the body’s tissues, causing inflammation and organ damage. This may affect your skin, heart, lungs, brain, and digestive tract.
HES can occur in people of all ages, but it is most common in individuals assigned male at birth between the ages of 30 and 50.4 Various factors may trigger the development of HES, including genetics, parasitic infections, drug hypersensitivity, blood cancers, and immunodeficiency disorders.
The symptoms of HES are determined by the organ system involved but commonly present with skin rash, fever, fatigue, muscle aches, weakness, and weight loss. The treatment of HES is directed at reducing the number of eosinophils in the blood and may be through corticosteroids, chemotherapy drugs, or targeted therapies, depending on the cause.
Types
- HES can be classified on the basis of etiology. Knowledge of which kind of HES you have leads to proper therapy.
- Myeloid hypereosinophilic syndrome: Arises as a result of the overgrowth of myeloid cells in the bone marrow causing overproduction of eosinophils.
- Lymphocytic variant hypereosinophilic syndrome: It occurs as a result of the overgrowth of abnormal T-lymphocytes (a form of white blood cell).
- Overlapped hypereosinophilic syndromes: Involve eosinophilic syndromes localized to a single organ system including EGPA as well as feature overlapping with IHES.
- Associated hypereosinophilic syndromes: It presents as a secondary complication of identifiable HES inducers, like parasitic infestations, drug hypersensitivity, or predisposing immune deficiency.
- Familial HES: This is caused by a few specific genetic mutations that can be inherited within families.
- Idiopathic: If there is no identifiable cause for eosinophilia, HES is referred to as “idiopathic,” a term used to describe a spontaneous condition or a condition that doesn’t have an identifiable cause
Symptoms of hypereosinophilic syndromes depend on which organs and tissues become targeted by excess eosinophils. Common symptoms include all types of HES such as:
- Red, itchy bumps (urticaria/hives) or swollen lumps under the skin called angioedema
- Fatigue
- Fever
- Pain in the muscles
- Weakness
- Loss of appetite and unintentional weight loss
- Cough
- Shortness of breath
- Memory problems
- Confusion
What Causes HES?
A normal eosinophil blood count is less than 500 cells per microliter (mL) of blood—typically less than 5% of all white blood cells circulating in your blood.Temporary increases in eosinophil counts can occur when your body is fighting a parasitic or viral infection or during an allergic reaction.
Hypereosinophilic syndrome is defined as eosinophils count of over 1,500/mL for six months or more.The exact cause of hypereosinophilic syndrome cannot be known; however, genetic mutations and primary diseases may also be contributing factors.
Gene Alterations
Gene alterations can result in hypereosinophilic syndromes through gene fusions and inherited gene mutations.
- Gene fusions occur when two previously distinct genes combine into one hybrid (fusion) gene with characteristics of both original genes. In HES, the fusion of the FIP1L1 and PDGFRA genes results in the production of proteins that initiate unchecked proliferation of eosinophils
- The gene mutations are hereditary and primarily pass down through families. Familial HES is caused by mutation in the 5q31-q33 region of chromosome 5, leading to an abnormality of the levels of a pro-inflammatory cytokine called interleukin-5, thereby controlling growth and mobilization of eosinophils.
Underlying Conditions
There are some underlying conditions that activate immune cells. This leads to the release of inflammatory substances from your body, which can result in overproduction of eosinophils. These conditions include:
- Parasitic, fungal, and viral infections
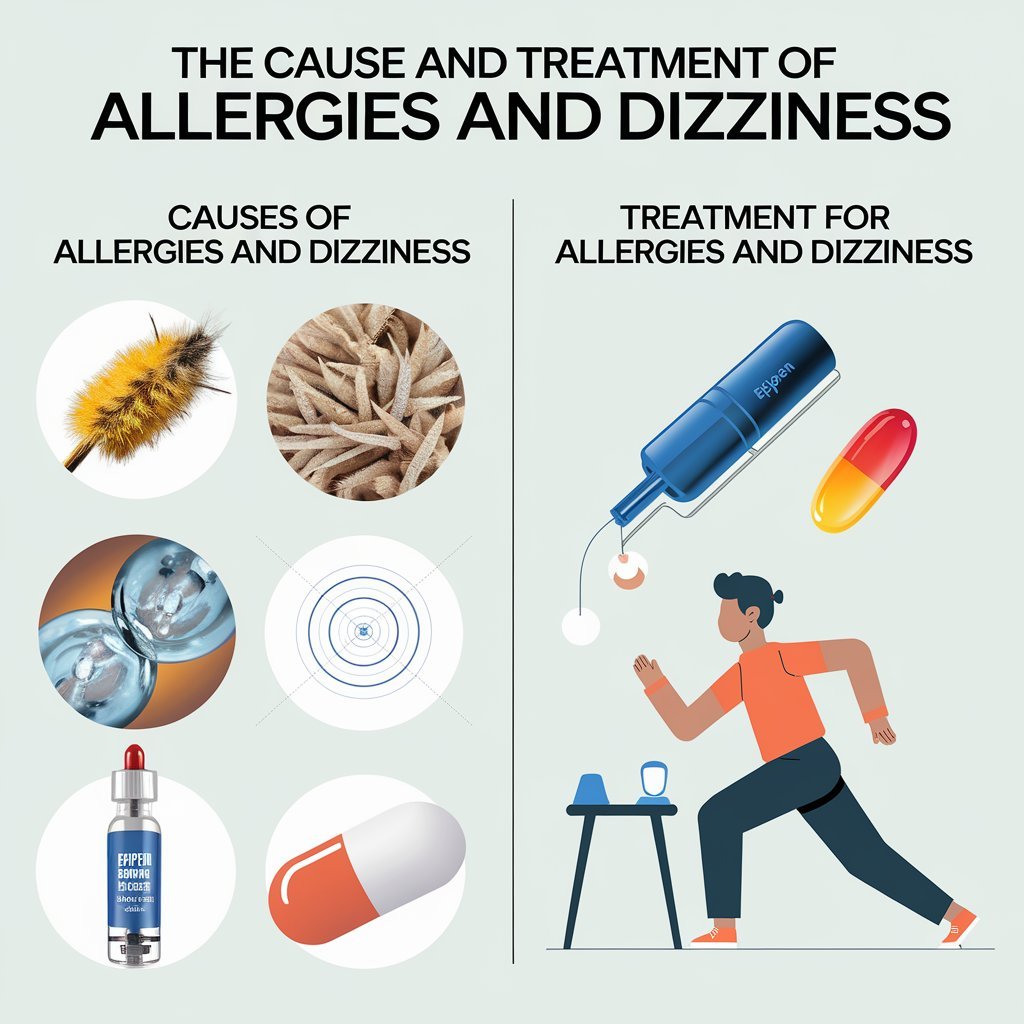
- Allergic reactions and allergy-related disorders, including asthma and atopic dermatitis
- Autoimmune disorders, including inflammatory bowel disease (IBD) and connective tissue disorders
- Blood cancers, including leukemia and lymphoma
- Drug hypersensitivity (allergic reaction to over-the-counter or prescription medications or dietary supplements)
Risk Factors
Anyone can suffer from hypereosinophilic syndrome, but the age of patients ranges between 30 and 50 years in most people assigned male at birth.
Diagnosis
Diagnosis of hypereosinophilic syndrome is usually hard since it is presented by a range of symptoms similar to other conditions like autoimmune diseases and allergic reactions. It often follows a stepwise procedure that attempts to exclude any other causes for your symptoms before HES is confirmed.
The provider will take your medical history including medications, past infections, present medical conditions, and family history. Your symptoms will be asked about and a physical examination conducted to detect signs of HES, including skin rash or shortness of breath.
- Blood tests to check your complete blood cell count (CBC) and eosinophil count. Blood tests can also measure substances that monitor liver and kidney function, vitamin B12, and tryptase levels (an enzyme that contributes to allergic reactions).
- Other imaging scans include X-rays, computed tomography (CT scans), and ultrasounds. In these imaging scans, your healthcare provider allows them to view your internal organs to check if there’s damage. For instance, a chest X-ray may show lung damage, while an echocardiogram-ultrasound means how your heart is functioning.
- Skin biopsy: This may be used to determine the cause of a rash. The provider may take a small sample of your skin and send it off to the lab for a technician to study under a microscope for the presence of eosinophils in the tissue.
- Bone marrow biopsy, where a small portion of the bone, usually taken from the hip bone, is extracted to check for abnormalities in white blood cells and determine the level of eosinophils in the bone marrow.
- Allergy testing through skin prick or blood tests may help identify allergies to certain materials, such as pollen, and determine allergic diseases.
Treatment of Hypereosinophilic Syndrome
Treatment for HES aims at minimizing the numbers of high eosinophils in your blood, lowering inflammation to prevent organ damage, and slowing disease progression. The treatment your healthcare provider recommends will depend on the organs involved and the cause of HES.

Corticosteroids
The first-line treatments for HES are corticosteroids such as prednisone. Powerful anti-inflammatory medicines are used for suppressing the eosinophil product and reducing the inflammation to avert organ injury. Steroid therapy is potent and effective with 85% of patients recovering with normal or near-normal counts of eosinophils in their blood.
Corticosteroids do not treat HES, and eosinophil levels will rebound back to elevated when you stop the medication. Steroid use long-term can have side effects that include weight gain, mood swings, high blood pressure, and bone loss.
Interferon Alpha (IFNa)
Interferon Alpha (IFNa) is an immunomodulating medication, meaning it modifies your body’s natural immune response. They are administered by injection into fatty tissue under the skin 3 to 5 times a week.
INFa reduces HES symptoms but, at first, causes flu-like symptoms, like fever, joint pain, and muscle aches. These symptoms will eventually dissipate. Long-term administration of INFa provokes severe side effects: elevated liver enzymes, low blood cell count, depression and mood disorders, and heart attack.
Monoclonal Antibodies
Monoclonal antibodies are a class of biologic drug. They are artificial immune system proteins that can be administered to individuals with HES when other therapies fail. Two monoclonal antibodies are available to treat HES:
- Nucala (mepolizumab): It works by binding and inhibiting interleukin-5, which is a cytokine that regulates the growth of eosinophils
- Lemtrada (lemtuzumab): It works by binding to the CD52 protein on the surface of eosinophils and causing them to die.
Tyrosine Kinase Inhibitors
Tyrosine kinase inhibitors are enzymes that are involved in the activation of inflammatory immune cells. Tyrosine kinase inhibitors such as Gleevac (imatinib) may reduce eosinophil counts and control symptoms of HES with minimal side effects in patients with HES due to particular gene changes.
Chemotherapy
Chemotherapy drugs, including hydroxyurea, cyclophosphamide, vincristine, etoposide, and methotrexate, kill rapidly proliferating cells like eosinophils. These are very strong drugs with severe side effects (such as nausea, vomiting, hair loss, anemia, and increased susceptibility to infection), and they are generally reserved for the most severe cases of HES.
Preventions
The reasons behind hypereosinophilic syndromes are varied and complex, and nothing can be known to prevent this condition. If you have risk factors for or a related condition to HES, then regular follow-up visits with your healthcare provider as well as monitoring of your eosinophil levels may be of help in the early detection of HES. Tenable diagnosis and treatment may hence be of help to prevent wide-ranging damage to organs and slow disease progression.
Associated Conditions
Individuals with HES commonly have other health conditions, most of which are secondary complications of the body’s organs being invaded and damaged by eosinophils.
- Eosinophilic gastrointestinal diseases: Infiltration of the gastrointestinal tract with eosinophils can be associated with pain in the abdomen, nausea, vomiting, diarrhea, bloating, and loss of weight.
- Allergic diseases: Many individuals with HES have allergic diseases, including asthma, food allergies, and atopic dermatitis. Shared genetic factors and excessive inflammatory responses may play a role in the connection.
- Heart disease: Eosinophil infiltration can damage heart muscles and valves, leading to arrhythmias (irregular heartbeat), heart murmurs, thrombus (blood clots), mitral valve insufficiency, or heart failure.
- Organ enlargement: Eosinophils accumulate in specific organs, including the spleen and liver, and can cause inflammation and organ enlargement in patients with HES.
- Lung damage: The infiltration of eosinophils into lung tissues can lead to a decrease in lung function and cause respiratory symptoms such as shortness of breath, coughing, and chest pain.
- Lungs: Eosinophils can invade and inflame lung tissues, which causes respiratory distress, asthma, cough, and even interstitial lung disease. This may influence the working efficiency of your lungs and how efficiently they can take in oxygen.
- Neurological complications: The presence of eosinophils within the nervous system may lead to seizures, neuropathy, or encephalopathy (memory issues and confusion).
Living With HES
There is no cure for hypereosinophilic syndrome, but getting involved in your care and following your treatment plan can help keep symptoms at bay, slow disease progression, and avoid extensive organ damage and complications. For most people with HES, treatment allows them to live long, healthy, productive lives. Without treatment, HES can be fatal.
Symptoms of HES can cause a lot in your life, forcing you to modify your daily routines. Ask family and friends to support you when you are most difficult or approach your healthcare provider about your challenge. They could have resources they can refer you to or perhaps change your treatment plan if symptoms worsen.