The Centers for Disease Control and Prevention say a tick bite-related red meat allergy is a new public health problem in the United States.
Other health issues tick bites can cause include Lyme disease, Rocky Mountain Spotted Fever, and Babesiosis. However, two new reports from the CDC show that alpha-gal syndrome (AGS)—a red meat allergy that starts with a tick bite—may have affected as many as 450,000 people in the U.S.
AGS’s symptoms include itching, rash, indigestion, nausea, and vomiting after the consumption of meat or dairy products. Some patients with this disease may even develop anaphylaxis, an extreme allergic reaction affecting multiple organs and potentially being life-threatening.
Between 2010 and 2022, the CDC reported more than 110,000 suspected cases of alpha-gal syndrome, a number that is probably much lower than reality: many with symptoms never get tested.
It is not easy to determine how common AGS is in the United States without a national surveillance system. But experts predict that AGS cases are increasing, likely because of increased awareness as well as emergencies.
“This is probably not a new syndrome, but a newly-recognized syndrome. We’re still learning a lot about it,” Daniel Pastula, MD, MHS, the chief of neuroinfectious diseases and global neurology at the University of Colorado School of Medicine and Colorado School of Public Health, told Health.
How Can a Tick Bite Cause a Red Meat Allergy?
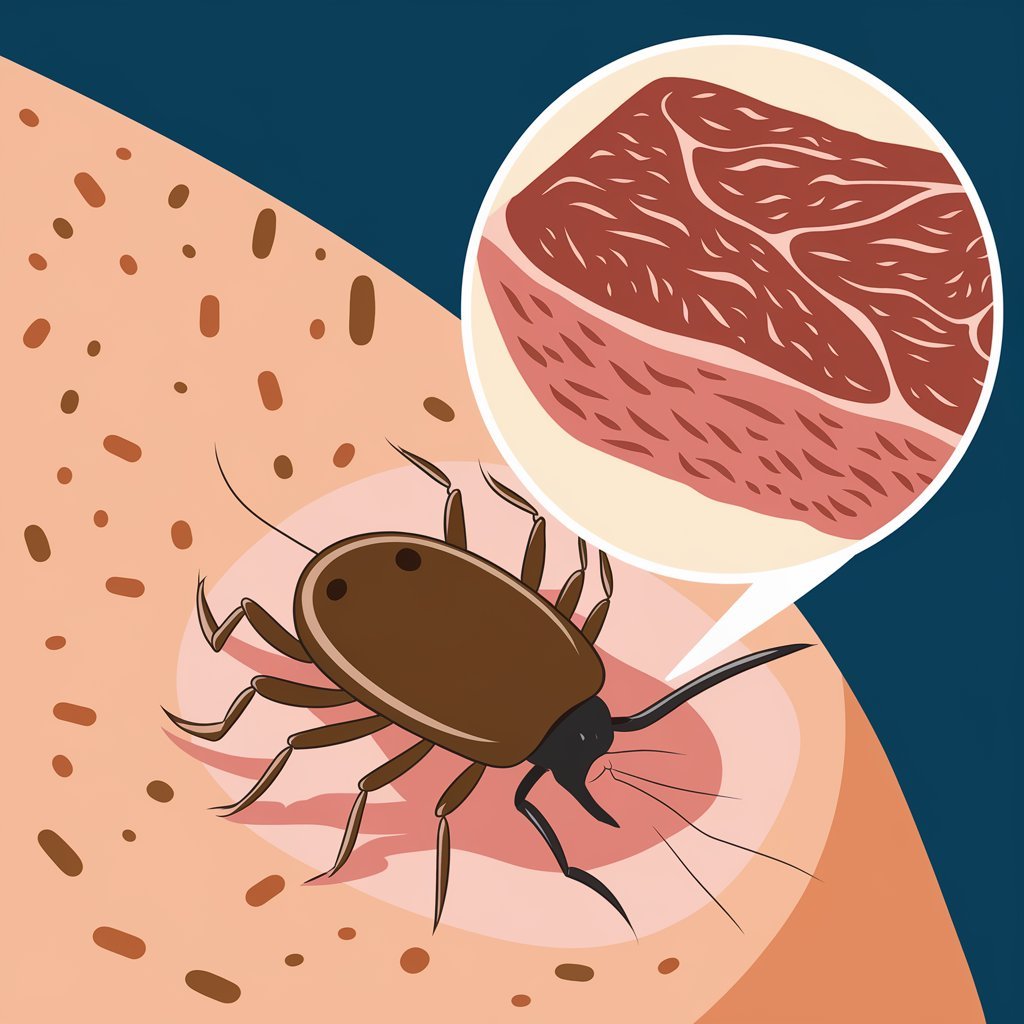
Scientists believe that, during a tick bite, tick saliva inoculates humans with alpha-gal sugar, which can trigger an immune response where the body produces antibodies against the sugar, according to Pastula.

This can lead to symptoms whenever a person ingests meat, such as pork, beef, mutton, lamb, venison, or another product, like gelatin, that contains alpha-gal.
In some people, the presence of alpha-gal in the blood triggers a reaction from the body’s immune system, resulting in an allergic reaction to alpha-gal sugar molecules,” Bobbi Pritt, MD, FCAP, a spokesperson for the College of American Pathologists and director of the Clinical Parasitology Laboratory at Mayo Clinic, told Health.
According to Pastula, not everyone who has been bitten by a tick and then produces antibodies against alpha-gal develops AGS. In fact, there are individuals who test positive for the antibodies against alpha-gal but never develop AGS.
Just because someone has a positive test result doesn’t mean they have the syndrome,” he said. “It just means they have antibodies against it.”
It is not known why only some individuals develop AGS following a tick bite, for example, or how long a tick needs to bite to trigger AGS.
“We don’t know all the details of what’s going on here,” said Pastula.
AGS Cases on the Rise, But Underdiagnosed and Under-treated
The CDC reports hundreds of thousands of Americans may be exposed to AGS.
Researchers at the CDC reviewed more than 350,000 specimens that were submitted by healthcare providers based on suspected cases of AGS. More than 30 percent of the submitted tests came back positive for antibodies against alpha-gal.
And it seems that the numbers are going up—the number of positive test results increased from 13,371 in 2017 to 18,885 in 2021.
Ann Carpenter, DVM, MPH, Epidemic Intelligence Service Officer at the CDC and primary author of one of the latest CDC reports, elaborated that the increase in the number of cases of AGS may be linked to the tick’s increasing range.

The lone star tick is found in the southern, midwestern, and mid-Atlantic United States. According to the CDC analysis, New York, Virginia, and Kentucky have reported the highest number of cases of AGS, while other states in these regions have also reported a high number of suspected cases.
The geographic distribution of AGS cases is similar to that of ehrlichiosis, a bacterial infection transmitted by lone star ticks.
According to Carpenter, the CDC hopes that this new report makes public health agencies and healthcare providers more aware of AGS hotspots so they can treat patients accordingly.
While the peak recent surge of cases of AGS has occurred where the lone star tick lives, 23% of the current crop of positive AGS patients come from a location where the lone star tick does not normally exist. A few of those patients admitted to being bitten by blacklegged ticks.
While other species of ticks are associated with AGS in other parts of the world, thus far, a large majority of cases occur in the United States, associated with the lone star tick.
Getting Healthcare Providers Up to Speed on AGS
Despite detection of AGS increasing, few healthcare providers have heard of it.
A more recent CDC report surveyed 1,500 family and general practitioners, internists, pediatricians, nurse practitioners, and physician assistants from around the nation and found more than 40% never have heard of the syndrome. And about one-third expressed a lack of confidence in how to diagnose and treat a patient with AGS.
This is the first national survey evaluating HCP knowledge and practices, said Carpenter. The findings are a call to action for improving patient care in the United States through HCP education.”.
As per Carpenter, the necessity for furthering healthcare provider education and awareness in the matter of AGS has a crucial role in accelerating and better accuracy of diagnosis regarding AGS patients’ treatment as well as knowledge regarding this newly arising epidemic condition and consequently in raising detection of the case.
Preventing Tick Bites Is a Key Way to Prevent AGS
The very best way to prevent AGS is to prevent tick bites. Being prepared is a helpful step toward accomplishing this goal.
According to Carpenter, prevention should be done by using Environmental Protection Agency (EPA)-registered insect repellents when stepping outdoors. Moreover, wearing pants and long-sleeved shirts would also prevent bites.
Tick prevention is particularly important when spending time in tick-prone areas, such as tall grasses, shrubs, and leaf litter, said Pritt.
After your outdoor activities, shower and check your body, clothing, and gear for ticks. If you’re spending several hours outdoors, Pastula recommends intermittently scanning your body for ticks.
If you find a tick attached to your body, you should use tweezers to remove it as soon as possible. Then, clean the bite area with soap and water or rubbing alcohol.
If you have AGS symptoms—that is, if you have an allergic reaction between two and six hours after eating meat—call a healthcare provider such as your primary care doctor or allergist. In order to diagnose the condition, a healthcare provider will need to perform a blood test that searches for antibodies against alpha-gal, conduct a physical examination, and collect information regarding your medical history.
“People with a diagnosis of tick-borne meat allergy can then be counseled on what foods to avoid in order to prevent potentially life-threatening allergic reactions,” Pitt said.
Though there is no treatment or cure, symptoms can be prevented by avoidance of meat, dairy, and other products with alpha-gal.
For some patients, avoiding tick bites for up to five years may lead to a decline in antibodies that cause allergic reactions, Carpenter said. New tick bites can reactivate AGS in some patients, and in some, AGS lasts a lifetime, Carpenter said.
“This is just another example that ticks are bad news and to avoid tick bites as much as you can,” Pastula said.