Allergic asthma is a chronic (long-term) breathing condition in which your airways become inflamed and narrow in response to inhaling allergens like pet dander, dust mites, and pollen. With allergic asthma, exposure to allergens triggers an overactive immune response, leading to symptoms of an “asthma attack” like coughing, wheezing, chest tightness, and dyspnea (shortness of breath).
Allergic asthma is the most common form of asthma, representing approximately 80% of cases of childhood asthma and 50% of cases of adult asthma. It’s a result of genetic and environmental factors. The treatment helps to control symptoms and lifestyle changes decrease the frequency of asthma attacks.
Allergic Asthma Symptoms

Allergic asthma symptoms will vary from patient to patient but can range from mild to extreme. Most cases of allergic asthma involve respiratory-related symptoms similar to those experienced with other types of asthma. Respiratory symptoms of allergic asthma, in addition, include allergy symptoms.
Respiratory Symptoms
When you breathe in an allergen, it inflames your airways, making them red and swollen. This can make you experience various respiratory symptoms that include:
- Wheezing : Whistling sounds when one breathes
- Coughing: A dry cough (not producing mucus)
- Breathlessness: Feeling one cannot breathe fully, or get adequate air into one’s lungs.
- Chest pain or tightness: An unpleasant feeling of tightness, pressure, or ache in the chest.
Allergy Symptoms
Those allergic asthma people usually experience allergy symptoms after some exposure to an allergen. These consist of:
- Runny or stuffy nose with clear mucus
- • Sneezing
- • Red, watery eyes
- Itchiness around the eyes, mouth, or nose
What Triggers Allergic Asthma?
In allergic asthma, your airways are overly sensitive to certain inhaled allergens such as dust mites, pollen, or pet dander. These substances are normally harmless but if you have allergic asthma, your body will see them as a threat and cause an overactive immune response.
Your immune system comes up with immunoglobulin E (IgE) antibodies that fight the perceived threat. These make your body release chemicals like histamine, cytokines, and prostaglandins that help in the inflammation process, thereby creating the symptoms of asthma such as shortness of breath and wheezing.
Genetics
More than 100 genes have been identified that increase your risk for developing allergic asthma. These genes affect aspects of your immune system and lung function, including:

Overactive immune response: Some genes regulate your immune system’s reaction to allergens. For instance, interleukin-4 (IL-4) and interleukin-13 (IL-13) are cytokines, which are substances that contribute to airway inflammation. Differences in genes that encode for these cytokines make you more prone to airway inflammation when you are exposed to allergens.
Epithelial barrier dysfunction: The epithelial barrier in your airways defends your body from environmental threats like allergens and infectious microbes (such as bacteria). Mutations in genes that determine how epithelial cells function disrupt how the barrier functions. As a result, allergens may more easily pass through your airways and lead to inflammation.
Function of smooth muscle: Differences in genes that help your smooth muscles work properly in your airways may contribute to airway hyperresponsiveness. That is, the smooth muscles in your airways contract more quickly in response to environmental triggers and cause your airways to narrow.
Environmental Triggers
Some individuals with allergic asthma develop symptoms in response to indoor or outdoor allergens. Common triggers for allergic asthma attacks or episodes include:
- Tree, grass, and weed pollen
- Pet dander
- Mold
- Dust mites
- Cockroaches (feces, body parts, saliva)
Risk Factors
Allergic asthma can occur at any age. The following factors can increase your risk:
- Family history: Having a family member with allergies or asthma increases your risk of allergic asthma.
- Early life exposures: Exposure to allergens and irritants in early childhood, such as secondhand smoke or dust mites, is associated with an increased risk of allergic asthma.
- Other allergic conditions: Allergic asthma is very common among those with other allergic conditions. The conditions include eczema-a group of chronic skin conditions which can cause inflammation, irritation, and swelling of your skin; and allergic rhinitis-commonly known as seasonal allergies.
- Socioeconomic factors: A low socioeconomic status increases the chances of suffering from allergic asthma. Higher residence in a rural area, increased exposures to allergens and airway irritants, and less access to healthcare may be among the potential factors
How Is Allergic Asthma Diagnosed?
Diagnosis of allergic asthma involves a complete medical history review and physical examination by a healthcare provider, either your primary care provider or an allergist. An allergist is a doctor who specializes in diagnosing and treating allergies, asthma, and other conditions related to your immune system.

You are asked questions such as how frequent your symptoms have been, and how severe and what provokes your symptoms. Examination of your eyes, ears, nose, throat, and skin and auscultation of the lungs for possible asthma-like wheezing occurs.
Diagnostic tests can actually confirm an allergic asthma diagnosis as they rule out other possible causes of your symptoms. They are as follows:
- Spirometry: Spirometry is a lung function test that makes you breathe into a mouthpiece attached to a machine called spirometer to observe how much air you can actually exhale through force from the lungs.
- Indirect bronchoprovocation. The clinician will then make you face direct allergic asthma provocateurs in this indirect sense to assess what precipitates airway reactivity to such provocative asthma allergen conditions.
- This form of bronchoprovocation is not performed outside of research institutions.
- Direct bronchoprovocation: You inhale a specific concentration of a substance such as methacholine, which causes bronchospasm (airway tightening). At a certain concentration of methacholine, this can be diagnostic of asthma.
- Fractional exhaled nitric oxide (FeNO) test: This measures the amount of nitric oxide in your breath when you breathe into a handheld device. It measures airway inflammation. The FeNO test is more often used to diagnose eosinophilic asthma-asthma caused by overactive white blood cells in your lungs
- Skin prick test: Your healthcare provider scratches a small amount of a potential allergen into the surface of your skin to determine if an allergic reaction, such as redness, swelling, or bumps, occurs in response to the substance.
- Blood tests: Immunoglobulin E (IgE) is the most common blood test. Immunoglobulin E is an antibody that your immune system produces in response to an allergen. High levels of IgE are present in the blood stream of the majority of allergic asthma sufferers.
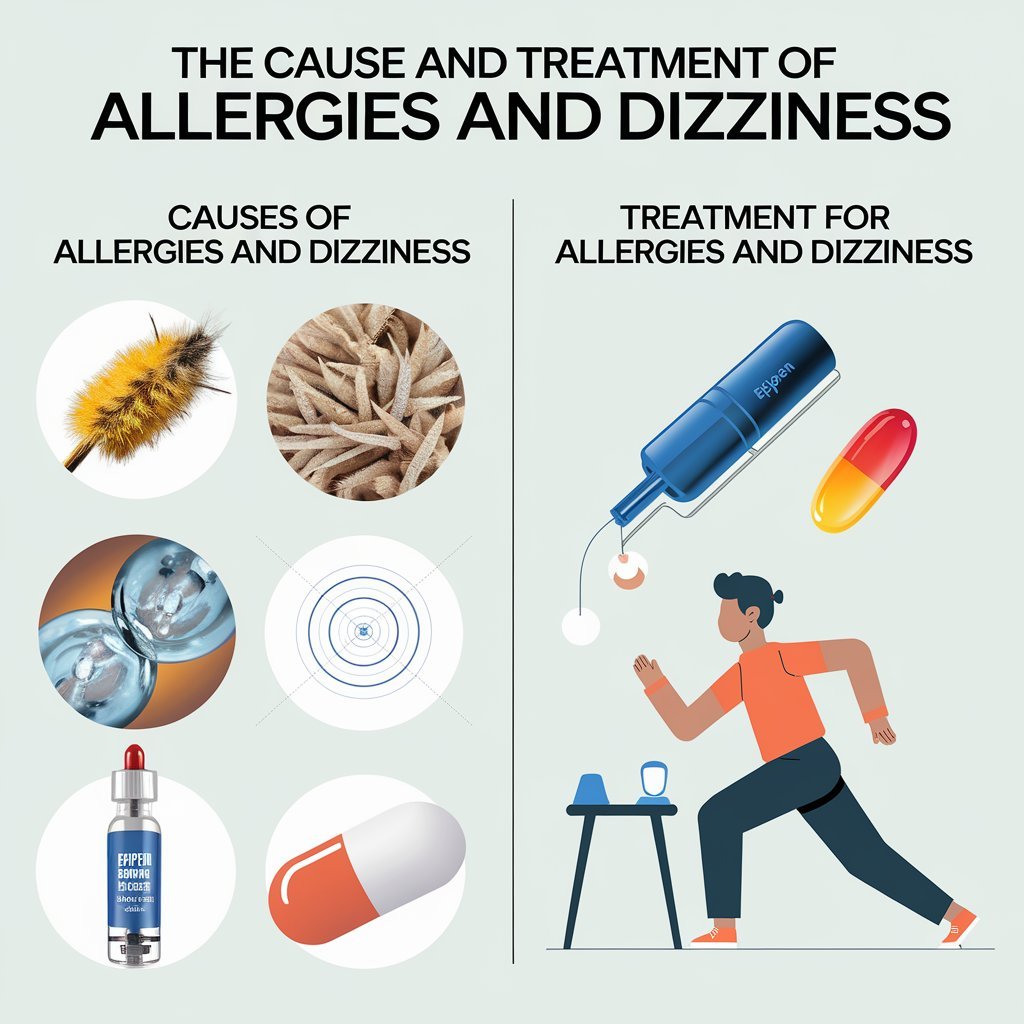
Treatments for Allergic Asthma
There is no cure for allergic asthma, but treatments can help manage symptoms. They can also keep your airways open to prevent future symptom flares (asthma attacks). Your healthcare provider will work with you to develop a personalized treatment plan, sometimes called an asthma action plan
Medications
Many medications reduce allergic asthma symptoms. Your healthcare provider may prescribe
- Quick-relievers are medicines that rapidly bring relief in case the allergic asthma symptom develops. It includes bronchodilators that are beta2-agonists and anticholinergics. They loosen up your airways, open them up and make breathing easy. These medicines are taken via inhaler or nebulizer to bring fast relief at the time of the development of the symptoms.
- Controller medicines: Medications taken daily can reduce inflammation and keep your airways open. Your healthcare provider may prescribe inhaled corticosteroids such as Flovent (fluticasone) or Pulmicort Flexhaler (budesonide). Oral anti-leukotriene medicines taken by mouth, such as Singulair (montelukast sodium), can block the action of immune chemicals that cause inflammation.
- Biologics: Biologics are medicines that contain a living substance. Some biologics target specific cells, proteins, and pathways that inflame airways. For instance, Xolair (omalizumab) blocks IgE antibodies that cause inflammation in the airways of individuals with allergic asthma.
- Antihistamines: Antihistamines block histamine—the chemical that causes allergy symptoms like runny nose, itchiness, and watery eyes.
- They’re available over-the-counter (OTC) and by prescription. Your healthcare provider may recommend using an antihistamine like Claritin (loratadine), Allegra (fexofenadine), or Zyrtec (cetirizine) when needed. They may recommend taking it daily to prevent allergy symptoms when your allergies are most severe (e.g., seasons with higher pollen levels).
Immunotherapy
Allergen immunotherapy helps build your tolerance to allergens. It reduces or eliminates your symptoms. Immunotherapy decreases your sensitivity and response to allergens like pollen, animal dander, dust mites, cockroaches, and mold over time.
The vast majority of allergy shots are required to be done on a regular basis, from once a week to once monthly. A treatment course is done for 3-5 years total. For the buildup phase, you receive shots weekly (3-6 months) before reaching the target dose. This is followed by the maintenance phase, where the shots are now given every 2-4 weeks for a duration of 3-5 years.
How to Prevent Allergic Asthma
- There is no way to prevent allergic asthma, but you can minimize the risk of attacks. Your healthcare provider will discuss these strategies with you as part of your asthma action plan:
- Identify and avoid triggers: This is one of the most effective ways to prevent allergic asthma attacks. It may include using allergy-proof bedding in order to limit dust mite exposure, installing air purifiers in your home, or checking local pollen forecasts and staying indoors during peak pollen times.
- Follow your treatment plan: Take your medications exactly as prescribed, even when you are symptom-free, to help control inflammation and keep your airways open.
- Use a peak flow monitor: Blowing into a small device called a peak flow monitor can help detect narrowing in your airways, sometimes before symptoms develop. It works similarly to how a thermometer measures body temperature. Your healthcare provider will let you know what your readings mean to help identify when to take quick-relief medicine, how much to take, and when you should call your healthcare provider or go to an emergency room visit for immediate medical care.
Related Conditions
Having allergic asthma may increase your risk of developing various conditions. These include:
- Atopic dermatitis (eczema): This is a chronic inflammatory skin condition that causes itchy, inflamed skin. It often develops before allergic asthma. The two conditions share many links, including allergen sensitivity, immune system dysfunction, raised IgE levels, and genetic factors.
- Sinusitis: Allergic asthma also leads to acute (short-term) or chronic sinusitis. Sinusitis is inflammation of your sinuses – air-filled cavities near your nose, eyes, cheeks, and forehead. It provokes mucus formation in your nasal passages and worsens asthma symptoms.
- Gastroesophageal reflux disease (GERD): GERD is a condition in which stomach acid flows back into your esophagus, a muscular tube that helps move food and liquid from your throat to your stomach. It causes symptoms like heartburn. Asthma can trigger the development of GERD and vice versa. GERD can also worsen asthma symptoms such as cough and breathing difficulty.
- Obesity: Obesity is related to chronic inflammation; researchers have projected that it may cause inflammation in the airway and contributes to asthma. Some allergic asthma medications, such as corticosteroids, can get less effective as well as the chance of having more severe symptoms increase with excess body fat.
- Living with allergic asthma is a really frustrating and, sometimes frightening situation. It’s a chronic illness that has to be constantly followed up with appropriate management; yet it needn’t determine your quality of life. With the right treatment strategy, it becomes a controllable condition.
- Well-controlled asthma means you can wake up in the morning, go about your daily activities, exercise without symptoms, and sleep through the night without the need for quick-acting medication. In short, you can lead an active and fulfilling life by working closely with your healthcare provider, actively managing your triggers and symptoms, and following your treatment plan.
- Discuss your treatment plan with your healthcare provider if you feel that it is not effective or if you experience a change in the symptoms of the disease.